The Brain
Experiencing a stroke or aneurysm is a life-threatening emergency requiring immediate medical attention. To help protect yourself or a loved one, it’s important to understand the risk factors as well as the symptoms of these conditions.
Ashish Masih, M.D., a vascular neurologist at INTEGRIS Health in Oklahoma City, explains that there are two broad categories of stroke – hemorrhagic and ischemic – and they are diametrically opposite conditions.
“Hemorrhagic is characterized by too much blood within the closed cranial cavity, while ischemic is characterized by too little blood to supply an adequate amount of oxygen and nutrients to a part of the brain,” says Masih. “An aneurysm is an abnormal bulge or ballooning in the wall of a blood vessel, and an aneurysm can burst. This is called a rupture of the aneurysm and results in a subarachnoid hemorrhage – which is a type of stroke. Genetics, hypertension, cigarette smoking and alcohol consumption are risk factors for aneurysmal development.”
He says the risk factors for stroke can be categorized as modifiable and non-modifiable.
“Age, sex and race/ethnicity are non-modifiable risk factors for both ischemic and hemorrhagic stroke like aneurysmal subarachnoid hemorrhage,” he says. “While hypertension, smoking, diet, diabetes, high cholesterol and physical inactivity are among some of the more commonly reported modifiable risk factors. I would recommend controlling all the modifiable risk factors that one can – and please stop smoking if you are smoking.”
Unfortunately, Masih says a subarachnoid hemorrhage is associated with a high early mortality rate.
“Population-based studies found that 18 to 24% of patients with a subarachnoid hemorrhage died suddenly prior to even being evaluated in a hospital,” he says. “In patients with ischemic strokes, prognosis varies from 10 to 26% in different populations.”
To help identify the symptoms of a stroke, the American Stroke Association encourages everyone to learn the F.A.S.T. warning signs.
F = Face Drooping: Does one side of the face droop, or is it numb? Ask the person to smile. Is their smile uneven?
A = Arm Weakness: Is one arm weak or numb? Ask the person to raise both arms. Does one arm drift downward?
S = Speech Difficulty: Is speech slurred?
T = Time to call 911.

Other stroke symptoms can include numbness on one side of the body, confusion, trouble speaking and/or walking and a severe headache with no known cause. When a person is suffering from a stroke, every minute counts. Receiving immediate medical attention can help minimize the long-term effects of a stroke and help prevent death.
The Ears, Nose and Throat
Sinus infections and ear infections can cause a lot of pain and discomfort, and often have similar symptoms. Jeremy Foon, M.D., M.P.H., an otolaryngologist/head and neck surgeon with Eastern Oklahoma Ear Nose and Throat in Tulsa, says it can be hard to tell the difference between the two infections without having a physician check the ears and nose.
Symptoms of a sinus infection can include headache, facial pressure, discolored mucus drainage, nasal congestion, fatigue and a poor sense of smell – while an ear infection can cause ear pain and drainage, difficulty hearing and tinnitus.
“The most common ear infection in adults is an outer [ear canal] infection also known as swimmer’s ear,” says Foon. “This can be related to swimming, but is also common when the ear is exposed to moisture and humid air. This is not the same as otitis media – a middle ear [behind the eardrum] infection – which is the most common ear infection in young kids. Kids in general are not more likely to get an ear infection from water exposure, despite common thinking.”



Foon says the number one ‘maintenance’ medication to help with chronic allergies and sinus infections is a daily intranasal steroid spray like Flonase or Nasonex.
“There is a common misconception that nasal steroid sprays can’t be used long-term,” he says. “This is not true! They can be used daily and for most people, indefinitely. Intranasal steroids do not spread to the rest of the body but instead stay confined to the nose. The daily nose sprays to avoid are decongestants, like Afrin. These are highly addictive and can damage the nose over time.”
In regard to the overall health of your ears, Foon stresses that the ears are ‘self cleaning.’
“That means for most of the population, leave them alone!” he says. “Q-tips, irrigations and home ear cleaning kits can often create more problems than solutions, like a blown eardrum. Q-tips are a major issue, because they push wax further in but don’t pull it out.”
In addition, he says keeping the ears dry with ear plugs or using swimmer’s ear drops is not usually necessary except in individuals who are predisposed to getting outer ear infections.

The Eyes
It’s smart to protect your eyesight at any age in order to prevent vision loss – and a few simple steps can make all the difference. An easy place to start is eye wear.
Ben J. Harvey, M.D., is a glaucoma specialist and clinical associate professor with the Dean McGee Eye Institute and the University of Oklahoma in Oklahoma City.
“Protecting your eyes from UV radiation in sunlight is important as it may exacerbate certain eye diseases like macular degeneration and cataract progression,” he says. “A brimmed hat is not sufficient; instead, polarized sunglasses are recommended.”
He also emphasizes that protective eye wear is largely underutilized.
“It’s vital to wear protective eye wear during any occupation or hobby that may create projectiles such as yard work, landscaping, woodwork, metal work, hammering and sawing,” says Harvey.
In addition, he says sleeping in contact lenses dramatically increases one’s risk of developing a vision-threatening corneal ulcer.

“Avoiding smoke and second-hand smoke can also reduce the risk of certain eye diseases progressing,” he says. “And excessive screen time is associated with development of myopia or nearsightedness in children, and it can exacerbate dry eye symptoms.”
Harvey says any time someone experiences a significant change in vision, increased redness or presence of eye pain, they should have a thorough ophthalmic examination.
“Certain conditions like diabetes require regular eye exams, and those with a family history of eye diseases should get checked by an ophthalmologist regularly as well,” he says. “For routine screening of eye diseases, the American Academy of Ophthalmology recommends everyone receive at least one comprehensive eye exam at least by age 40 and approximately every year after age 65.”
Harvey, who also specializes in treating cataracts, says cataract surgery has one of the highest impacts on quality of life compared to any other surgery.
“More recent advancements in specialty intraocular lens implants have the potential to further augment one’s quality of life by increasing one’s independence from glasses,” he says. “Such lenses can be tailored to individual patients to accommodate their lifestyle.”
However, he says to be sure and talk to your ophthalmologist about your options.
“Not everyone is a candidate for these specialty lenses, and some may be contraindicated in certain conditions – and no lens implant can currently guarantee spectacle independence,” he says.
The Heart
David Sandler, M.D, a cardiologist with the Oklahoma Heart Institute in Tulsa, says “despite significant medical advances and accessible health and wellness resources, someone dies from cardiovascular disease every 34 seconds in the United States.” And while a family history of heart disease can increase one’s risk of cardiovascular disease, obesity and diabetes are the largest contributors.

“You can reduce the risk [of heart disease] with exercise, a healthy and balanced diet, limiting alcohol consumption, avoiding smoking and vaping, and keeping your blood pressure and cholesterol levels at proper levels,” says Sandler. “In our office, we offer screening tests for people to become more proactive with heart disease. These include ultrasounds, stress tests and CT scans. These tests can help predict susceptibility to cardiovascular disease, but do not negate the importance of adopting a healthy lifestyle.”
In recent years, studies have shown an increase of diabetes and obesity in young adults aged 20 to 40 years old, which can affect one’s overall risk of heart disease now and later in life.
“The younger you are when you develop conditions such as diabetes and hypertension, the more likely you are to develop heart disease in your lifetime,” says Khaldia Khaled, M.D., F.A.C.C., F.S.C.A.I., an interventional cardiologist with the CardioVascular Health Clinic in Oklahoma City. “Knowing you have risk factors and are predisposed to conditions helps treatment planning. Having a family history of heart disease is a well-known risk factor for coronary artery disease, especially a family history of premature coronary heart disease. These are the patients that we want to catch early and optimize medically. We can’t change someone’s family history of heart disease but we can perform early screening and treat for things like hypertension and diabetes in their early stages to help prevent the negative impact they have on cardiovascular health.”
If you’re facing these risk factors, Khaled recommends finding a primary care provider that you’re comfortable with and working towards mitigating your risks.
“We should start teaching children at early ages about exercise and healthy eating,” says Khaled. “When you grow up exercising and eating healthy regularly, those habits and patterns are more likely to cross over into adulthood. These are the ‘lifestyle modifications’ we often try to implement too late in life.”
The American Heart Association recommends at least 150 minutes per week of moderate-intensity aerobic exercise or 75 minutes per week of vigorous aerobic activity, or a combination of both.
“Activities that elevate your heart rate can include brisk walking, jogging, sprinting, swimming, weightlifting, pickleball, tennis and basketball,” says Sandler. “I recommend a combination of cardio and weight training to develop strength, reduce body fat and preserve proper range of motions and mobility. Spread your activity over the week and do something every day. Ideally, find an activity you can truly enjoy, but it’s important to prioritize exercise, even if you don’t find every activity ‘fun.’”

Sandler, who also specializes in heart rhythm disorders, regularly treats patients with heart arrhythmias – meaning the “heart beats irregularly, too fast or too slow, including short-lived feelings of the heart fluttering, thumping or pounding.”
He says the complexity of arrhythmias lies in the fact that they can go undetected.
“Some experience no symptoms while others may feel one or more of the following: palpitation, skipped heart beats, heart racing, weakness, dizziness, lightheadedness, fainting and shortness of breath,” he says. “Since heart rhythm abnormalities can lead to stroke, congestive heart failure, and death in severe cases, I recommend keeping track of your heart rate with personal devices, such as an Apple Watch and scheduling time with a doctor to review abnormalities you may discover. If your device has the capability, it is very useful to record an ECG strip and print it for your doctor to review.”
The Lungs
According to the American Cancer Society, lung cancer is the leading cause of cancer deaths in the United States, accounting for about 1 in 5 of all cancer-related deaths.
Mark Boomer, M.D., a pulmonologist with Saint Francis Health System in Tulsa, says an early diagnosis is key to more positive outcomes.
“If a patient is in stage 1A cancer and they have surgery to remove the cancer, their five-year survival rate is 92%,” says Boomer. “Unfortunately, this past year, the national survival rate for lung cancer was 21%.”

He says there are multiple factors influencing these numbers.
“One of the reasons that lung cancer is such a silent killer is that there are no early symptoms,” says Boomer. “Once a person is manifesting symptoms, it’s often too late – the disease is at an advanced stage.”
He says with current healthcare shortages in many areas across the country, the time frame between receiving a screening, biopsy and diagnosis, can sometimes be longer than a patient should wait. In addition, local and national rates of lung cancer screenings are dismally low.
“Last year in Oklahoma, 1.7% of eligible patients were screened and nationally, only 4.5% of eligible patients were screened,” says Boomer. “I believe we can do better. One of the things that worries me about lung cancer and screening rates is that new data is showing the incidence of lung cancer in nonsmokers is going up, and we don’t know what’s causing that.”
The U.S. Preventive Services Task Force currently recommends annual lung cancer screenings for people who are ages 50 to 80 years old, have a 20 pack-year smoking history, and who currently smoke cigarettes or have quit smoking within the past 15 years.
“People under the age of 50 do get lung cancer, but it’s rare,” says Boomer.
Regarding risk factors, it’s commonly known that smoking cigarettes increases one’s risk of lung cancer, however, the effects of long-term vaping are still relatively unknown.
“The lungs were designed to breathe air,” says Boomer. “Any form of smoke, including vaping, is bad, whether it’s smoke from cooking over an open campfire, smoking meats on the barbecue, or smoking marijuana. We don’t know the long-term effects of vaping because we haven’t had a generation of people who have vaped for 30 or 40 years. We know there are products that contain noxious toxic chemicals and that even young patients have suffered acute lung injuries and ended up on ventilators; it’s rare, but it happens. Vaping was originally designed to get people off cigarettes and then in turn, get them off vaping. But it hasn’t been utilized that way, and that’s the problem.”
He says with smoking, if you smoke a pack a day and you quit smoking at age 40, it adds an average of seven years back to your life. But with vaping, there’s not enough studies to provide these types of statistics.
Despite the need for increased awareness regarding lung cancer and screenings, Boomer shares the encouraging news that within the field of pulmonary oncology, there have been significant medical advancements in care.
“In the last five or 10 years, there’s been the development of many new treatment options,” says Boomer. “There are new chemotherapies, immunotherapies, genetic therapies and new ways to diagnose lung cancer.”
To learn more about your risk for lung cancer, take a simple online screening, or schedule a screening, visit saintfrancis.com/lungscreening.
Critical Care
Tulsa’s only ACS (American College of Surgeons) nationally verified Level II Trauma Center can be found at Ascension St. John Medical Center, which delivers advanced critical care for the community – when it’s needed the most.
On-call 24 hours a day and seven days a week, trauma surgeons, neurosurgeons and orthopedic surgeons make up the expansive team that saves lives. Other surgeons specializing in cardiothoracic, vascular, hand, plastics, obstetrics/gynecology and urology cases are also available at all hours.
“I am so proud to work with a team that dedicates themselves to caring for our community’s most critically-injured patients every day,” says Ascension St. John Health System CEO Bo Beaudry. “When it comes to trauma care, we strive to hold ourselves to the highest standards possible, which means we are delivering high quality care to those that need it most, when they need it most, right here in Tulsa.”
While the ACS-verification process is voluntary, it validates the resources available for trauma care at trauma centers, which ultimately provides an organized and systematic approach to the care of injured patients. According to the ACS, Level II Trauma Centers must have 24-hour immediate coverage by specialty trained trauma surgeons, as well as orthopedic surgery, neurosurgery, anesthesiology, emergency medicine, radiology and critical care specialists. Ascension St. John has been ACS-certified since 2009.
The Trauma Center delivers advanced critical care to help stabilize, diagnose and treat a broad array of trauma, including:
- Blunt force trauma, including falls and personal injuries
- All penetrating trauma (including ballistics injuries and piercing wounds)
- Motor vehicle crashes, including cars, motorcycles, ATVs and bikes
- Multiple severe fractures
- Severe falls, including broken hips
- Spine injuries
- All brain injuries, including the most severe
The Stomach
Approximately 10-15% of people in the United States have irritable bowel syndrome (IBS) and nearly twice as many women than men have the condition, according to the American College of Gastroenterology. Symptoms of IBS, which include constipation, diarrhea, gas and bloating, can cause patients to miss out on daily activities.
“Patients with irritable bowel syndrome also frequently have nonulcer dyspepsia, also known as functional dyspepsia,” says William Tierney, M.D., a gastroenterologist with OU Health in Oklahoma City.
Functional dyspepsia refers to symptoms of an upset stomach or chronic indigestion, but with no obvious cause. It is part of the spectrum of functional bowel disease which includes irritable bowel syndrome, functional abdominal pain and functional heartburn.
“There are upper GI [gastrointestinal tract] symptoms, but when we look for signs of inflammation or disease, we don’t find any objective evidence of disease because IBS and nonulcer dyspepsia falls under the category of functional bowel diseases.”
With functional bowel diseases, Tierney explains that patients have clear symptoms of GI distress but without the inflammation that’s associated with inflammatory bowel disease, such as Crohn’s disease and ulcerative colitis.
“These patients may have an upper or lower endoscopy or perhaps a panel of blood tests, but there will be no signs of disease or inflammation,” he says. “Instead, we think there’s an alteration of the normal physiology of the GI tract – the visceral nervous system of the gut and motility of the digestive system is altered in these patients.”
Tierney notes that there’s been some improvement in understanding functional bowel disease, specifically regarding individuals whose symptoms may be caused by changes in the bacteria of the digestive tract.
“It’s a very small percentage of cases, but it’s worth investigating,” he says. “One condition in particular is small intestinal bacterial overgrowth where there is excess bacteria in the small intestine that leads to a lot of gas formation as well as diarrhea and/or constipation and bloating. We’ve found that if we treat patients with certain antibiotics to get rid of the unhealthy bacteria, then symptoms improve.”
Tierney says younger adults present the most incidents of functional bowel disease but it can occur at any age.
“While functional bowel disease can even begin in childhood, the older a patient is, especially in older adults, there’s greater concern that symptoms could be related to more serious causes such as stomach or colon cancer,” he says.
Tierney says another condition that’s gaining attention is metabolic dysfunction-associated steatotic [fatty] liver disease (MASLD) – previously known as non-alcoholic fatty liver disease. This disease occurs when the body begins storing excess fat in the liver and is often associated with other metabolic disorders such as high cholesterol, diabetes and obesity.

“Over time, this accumulation of fat in the liver can lead to chronic inflammation, scarring/cirrhosis and liver failure,” he says. “MASLD is now becoming one of the most common reasons for liver transplantation in the country. With Oklahoma having very high rates of obesity, we’re seeing a large number of patients with this particular condition. The mainstay of treatment for MASLD is weight loss and exercise.”
With the many varied and complex conditions related to the body’s digestive system, individuals should never ignore symptoms.
“We are seeing more and more young people with colon cancer, patients in their 30s and 40s,” says Tierney. “As a result, we recommend even young patients take symptoms such as blood in their stools seriously and undergo a colonoscopy. It’s why it’s so important for individuals to work with their primary care physician or digestive disease specialist to determine a diagnosis and manage treatment, particularly if there are high risks signs of bleeding or weight loss.”
In regard to advances in the field of gastroenterology, he says there have been a number of very impactful innovations.
“Advancements in procedures, such as in interventional endoscopy now allow patients to undergo less invasive procedures to treat or cure disease that in the past would require a major surgery,” says Tierney. “In addition, new medications have revolutionized the care of patients with inflammatory bowel disease and certain liver diseases such as viral hepatitis C. In the era of artificial intelligence, we are already seeing an impact on improving the quality of care for patients undergoing colonoscopy and we will certainly see further AI advances in disease diagnosis and optimizing medical management. It’s really an exciting time to be in the field.”
The Joints
Being active and moving freely without chronic joint pain significantly impacts a person’s quality of life. It’s estimated that more than 700,000 Americans receive total knee replacements each year, both to treat pain and stay mobile.
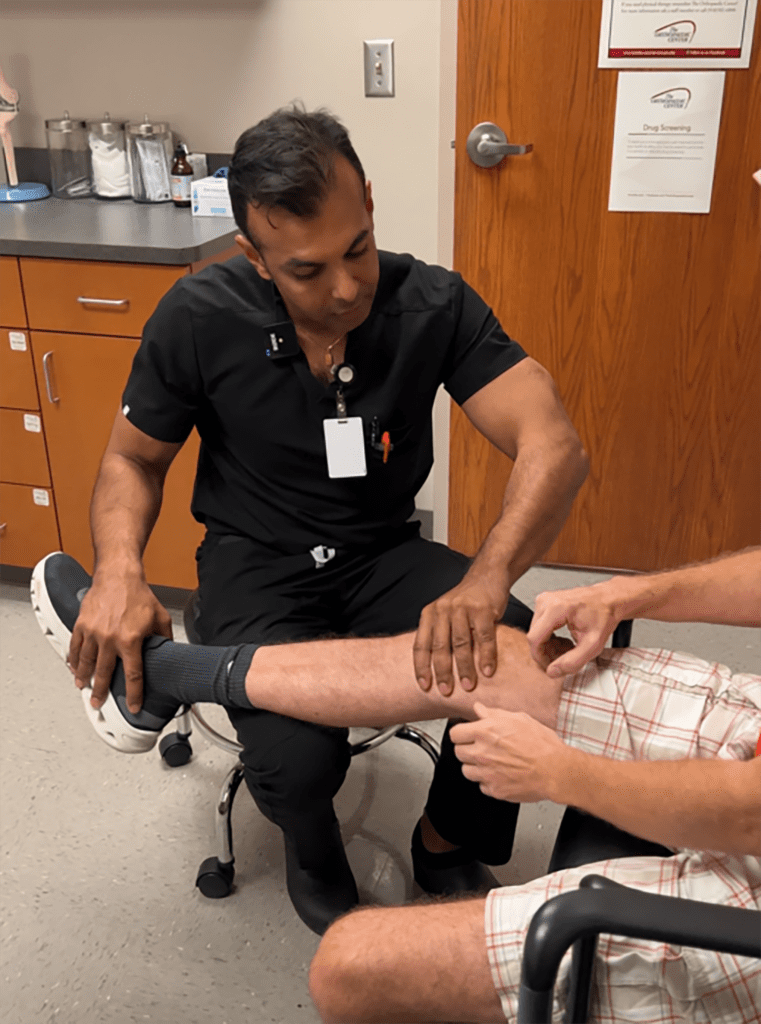
Yogesh Mittal, M.D., an orthopedic surgeon with The Orthopaedic Center in Tulsa, says the most common reasons patients receive a knee replacement are pain, lack of mobility and a decrease in function, and the average age to have the surgery is around 65.
“However, we are seeing more younger patients because we are more active as a society and surprisingly, also older patients in their 80s,” says Mittal. “We are living longer healthier lives, so our joints are wearing out.”
According to the American Academy of Orthopaedic Surgeons (AAOS), the most common cause of chronic knee pain and disability is arthritis, such as osteoarthritis, rheumatoid arthritis and post-traumatic arthritis. The AAOS reports that currently more than 90% of modern total knee replacements are functioning well 15 years after surgery.
Mittal says the continued development of robotic and computer-assisted surgery has disrupted the medical field in a good way, and other notable advances include a greater emphasis on pain control to allow for less pain during rehabilitation.
“Because we get a CT scan prior to surgery, there is a substantial amount of pre-planning and customization of the implant positioning to that patient’s unique anatomy,” says Mittal. “Intra-operatively, we can balance the knee more precisely and the robotic system helps with decision making. Also with robotics, a robotic arm assists in cutting the bone much more accurately and safely, and can also be less invasive and potentially allow for quicker recovery.”
Once a patient recovers, they can typically enjoy an active lifestyle with few limitations.
“It’s O.K. to jog, but ideally, we do not want our patients to begin running long distances,” says Mittal. “Otherwise, I allow all other activities.”

Telemedicine
Telemedicine has been around for decades, but with the shift in healthcare needs throughout the pandemic and beyond, it’s become an essential service. In recent years, at both national and state levels, legislative changes have helped progress telemedicine by increasing the scope of services offered, improving provider reimbursement, and applying new security regulations to protect patient privacy.
According to a 2022 survey conducted by Stanford Medicine’s Center for Digital Health and Rock Health – a nonprofit that supports innovations in digital health – telemedicine reached an 80% adoption mark overall, becoming the preferred channel for prescription care and minor illnesses. Other notable changes within the survey results included an increased use of telemedicine by respondents over the age 55, respondents living in rural areas, and respondents without health insurance at the time of the survey.