The Brain
Signs of Dementia
“Dementia is an umbrella term,” says Jason King, M.D., a neurologist with Ascension St. John in Bartlesville. “There exists an array of dementing illnesses – vascular dementia, Lewy body dementia, frontotemporal dementia and Alzheimer’s dementia – and there can be ‘mixed dementia’ as well.”
The most common type in the U.S. is Alzheimer’s disease, which carries genetic risk factors.
“Studies have indicated that variations in the APOE gene can either reduce or enhance one’s risk of developing the disease,” says King. “If you are a carrier of the gene APOE2, you are at a slightly decreased risk, while if you carry the APOE4 gene, you are at a slightly increased risk. However, being a carrier of the APOE4 gene does not automatically guarantee you will develop Alzheimer’s disease. In terms of true, genetic Alzheimer’s which is directly inherited from a parent – this is extremely rare and has only been found in a few families worldwide.”
Personal behaviors can influence the risk.
“Recent studies indicate that strict control of ‘vascular’ risk factors such as high cholesterol, high blood pressure and diabetes are very important,” says King. “In fact, we have found that when blood pressure is most strictly controlled, normalized to 120/80, not merely just less than 140/90, risk of dementia can be significantly reduced.”
King says early symptoms of dementia vary by disease.
“For Alzheimer’s, it is the very short-term memory which is generally affected first; other cognitive domains are spared early on,” he says. “However, in frontotemporal dementia, executive function and personality changes can be seen in the early stages.”
Recognizing a Stroke
“Roughly 1.9 million brain cells die each minute during a stroke,” says Cameron Richardson, MSN, RN, ASC-BC, stroke program manager with Tulsa’s Saint Francis Health System. “That’s about 31,600 brain cells each second. With a blockage type stroke – ischemic – there is a core area of dead brain with an area around it that is at risk of dying – penumbra. For the bleeding type stroke – hemorrhagic – blood is touching the brain when it normally does not, and an area of the brain is not getting that blood flow.”
Stroke treatments are what potentially save at-risk brain tissue.
“Calling 911 is so critical because it’s the first step in the stroke chain of survival, which decreases the total time for someone to potentially receive treatment,” says Richardson. “Less time means less brain cell death. Time is brain.”
Richardson explains that the time frame from when a person was last feeling and acting normal helps guide which type of stroke treatment may be administered.
“However, we are in the middle of an exciting time of stroke research where there are the beginnings of a transition from only time guiding care to time and tissue,” he says. “That means how the brain looks on a scan can also guide treatment.”
The medical community encourages people to follow the acronym B.E.F.A.S.T. – for Balance, Eyes, Face, Arms, Speech, Time and Terrible Headache. While the majority of strokes aren’t painful, Richardson says the most deadly type of stroke, hemorrhagic, is commonly associated with a sudden, terrible headache.
People can also experience a transient ischemic attack (TIA), often called a ‘mini stroke.’ A TIA is a temporary blockage of blood flow to the brain, with symptoms lasting from a few minutes to up to 24 hours.
“The frightening thing about a mini stroke is the heightened chance of an actual stroke within the next year,” says Richardson.
He also shares the reminder that a stroke can happen to anyone.
“It isn’t just the middle aged and older or those with numerous risk factors,” he says. “We see marathon runners and football players. Children and young adults have strokes every year and often do not get treatment because they arrive to the hospital after 24 hours.”
Maxillofacial Health
In the field of oral and maxillofacial surgery, common procedures include wisdom teeth removal, placement of dental implants, and jaw surgery, also known as orthognathic surgery, says Christopher Ray, D.D.S., an oral surgeon with Eastern Oklahoma Oral and Maxillofacial Surgery (EOOMS) in Tulsa.
“Other related procedures include bone grafting or full mouth extraction in preparation for implants and implant-retained dentures,” he says.
Heath Evans, D.D.S., an oral surgeon and Ray’s colleague, says people may not realize the frequency or impact of corrective jaw surgeries.
“These are cases typically done in conjunction with orthodontics to correct jaw misalignment,” says Evans. “These patients have some of the most profound changes that we see, and these procedures can certainly be life changing.”
Ray shares that technological advancements in imaging have facilitated better surgery planning.
“We use digital intraoral scans and cone beam computed tomography (CBCT, 3D scanning) in conjunction with planning for orthognathic surgery as well as complex full replacement dental implant cases,” he says. “We are able to merge hard and soft tissue data and digitally complete the surgery in order to fabricate splints, guides and other modalities to translate planning into practice.”
Evans offers assurances that comfort is a priority for his patients.
“Our ability to provide in-office anesthesia for qualified patients is a huge part of our practice, and oral and maxillofacial surgery,” he says. “This allows us to ensure patient comfort even in very challenging circumstances.”
The Eyes
The World of Oculoplastics
If you’ve not needed an oculoplastic surgeon, you may not be aware of the particular skill sets this field of medicine offers.
“Oculoplastic surgeons are ophthalmologists who are specialized in plastic and reconstructive surgery of the periorbital and facial tissues, including eyelids, eyebrows, orbit [eye socket] and lacrimal [tear] system,” says Thai Do, M.D., an ophthalmologist at Oklahoma City’s Dean McGee Eye Institute. “With extensive training, oculoplastic surgeons have the anatomical understanding and surgical finesse to treat complex conditions around the eyes.”
He says common cosmetic procedures performed by oculoplastic surgeons include blepharoplasty (removal of excess eyelid skin), ptosis repair (droopy eyelid lifting), endoscopic forehead and brow lift, mid-face lift, herniated orbital fat removal and injectables.
Jeremy Tan, M.D., an ophthalmologist and Do’s colleague, says there are standard approaches to a blepharoplasty and a brow lift, but each patient’s anatomy is unique.
“For instance, addressing the upper eyelid crease in the Asian eyelid is one of the most challenging aspects of upper eyelid surgery – there may need to be a reinforcement, or sometimes complete creation of this fold,” says Tan. “In lower eyelids, fat pad prolapse in relation to the position of the globe [eyeball] presents certain challenges for maintenance of lower eyelid height. Finally, the weight of forehead tissues and hairline height are taken into consideration for the type of brow lift that is offered.”
Do says eyelids and periorbital tissues are some of the body’s most complex and intricate structures.
“These structures serve essential functions, including eyelid opening and closing, blinking, tear drainage and facial expressions, which can easily be impaired,” he says. “The margin of error for these surgeries is often in millimeters – sometimes a fraction of a millimeter.”
From a cosmetic perspective, Tan says the periocular region sets the stage for the visual mood of the face.
“The biggest compliment I get from patients after they have healed from a procedure is that their friends and family tell them they look ‘well-rested,’” says Tan. “From a functional standpoint, the upper eyelids and brows, when heavy and droopy, can block peripheral vision. Also, straining to recruit forehead muscles all day long, to lift droopy lids, can cause headaches. Our surgical interventions can help these issues directly and are a common benefit noted by our patients.”
Cataract Surgery and Corneal Transplantation
Many people find themselves faced with diminished vision, in need of cataract surgery or a corneal transplant.
“Cataract surgery technology continues to improve with respect to both safety and efficacy as biometric, microscopic and microsurgical equipment technologies continue to advance,” says Marc Goldberg, M.D., an ophthalmologist with The Eye Institute in Tulsa.
“Existing pre-operative and newer intraoperative measuring technologies have improved our lens implant selection accuracy dramatically, even over the past few years,” he says. “The improved accuracy of our measurements and the rapid evolution of ‘premium’ intra-ocular lens implant options (IOL’s), which can correct for astigmatism and also for simultaneous near and distance vision correction inside the eye, has elevated modern cataract surgery to the point that we can now consistently provide excellent uncorrected vision to most cataract surgery patients with a brief, usually painless and low-risk procedure.”
Goldberg says individuals who are good candidates for a corneal transplantation are those with abnormalities of corneal contour, corneal scarring or opacity, and persistent corneal edema or swelling.
“Corneal transplantation, also called keratoplasty, may be complete (penetrating) or partial thickness (lamellar) depending on the corneal disease type and severity,” he says.
The Heart
Cardiovascular disease remains the leading cause of death in the U.S., and an estimated 80% of cardiovascular diseases are preventable, according to the American Heart Association. To avoid joining the statistics, diet and exercise still reign supreme – but it’s a challenge for many.
“The biggest changes are often the easiest to make, on paper anyway, but oftentimes are the hardest to implement, as it requires a change in behavior,” says Mark Blubaugh, D.O., partner and medical director at Tulsa ER & Hospital.
He says a heart-healthy diet should include two to three helpings of fruits and vegetables at every meal and limiting red meat intake to once a week.
“This can be replaced with healthier animal proteins like chicken and fish or even substituting with plant proteins,” says Blubaugh. “Try to limit the amount of saturated fat and trans fat, along with the amount of sweets. While alcohol indulgence is not advised, a good rule of thumb for alcohol along with non-heart healthy foods is ‘everything in moderation.’”
Along with a healthy diet, exercise is key to strengthening the heart.
“Good cardiovascular exercise increases the heart’s ability to efficiently pump blood throughout the body and also decreases peripheral vascular resistance,” he says. “Both of these combinations will lead to increased cardiovascular health and better blood pressure.”
However, before kicking off any new routine, Blubaugh recommends visiting your primary care provider to assess your heart health and risk factors.
“This is especially true if you are high risk for cardiovascular disease,” he says.
The Lungs
While smoking cigarettes remains the No. 1 cause of lung disease and lung cancer, Sergio Garcia, M.D., a pulmonologist with Norman Regional Health System, says it’s still important to remember the effects of secondhand smoke exposure and other respiratory threats.
He often sees family members who have developed cancers, emphysema and worsened asthma due to secondhand smoke exposure.
He adds that individuals need to be aware of the dust and chemicals they are exposed to at work. Farmers are subjected to certain allergy-causing dust, pesticides and other chemicals that may cause lung disease. Those who work with dusts, ground metals and aerosolized cotton particles can be harming their lungs if they’re not careful to protect themselves.
“Of course, the environmental allergens, smog, temperature and weather can also affect the lungs,” says Garcia. “Even radon found especially in older buildings with basements can predispose us to lung cancer. The list of potential exposures is long.”
Fortunately, Garcia says new advancements in technology continue to expand treatment options for those suffering with lung disease and/or lung cancer.
“Numerous new inhalers that are used for lung disease, such as asthma and COPD, have been developed and improved over the last decade,” he says. “Newer diagnostic and therapeutic tools that use the latest in technology have been applied to interventional bronchoscopy to help detect, stage and treat lung cancers. Navigational bronchoscopy and robotic bronchoscopy are good examples, as well as endobronchial ultrasound.”
In addition, he says chemotherapy agents have changed significantly, and now genetic markers in certain lung cancer help guide the decision to choose the most successful therapeutic agent.
The Gastrointestinal System
Identifying Problems
William Tierney, M.D., an OU Health gastroenterologist and professor at the University of Oklahoma Health Sciences Center, says there are a number of digestive symptoms that warrant an evaluation by a gastroenterologist.
“Patients with longstanding heartburn, particularly if it is not responsive to over-the-counter remedies or is associated with difficulty symptoms such as a sense of food getting stuck in the esophagus or weight loss, should be evaluated by a specialist,” says Tierney. “Likewise, anyone with signs of bleeding from the digestive tract, which can be red blood in the stool or black stool, should be seen urgently.”
He adds that anyone with diarrhea that persists more than a couple of weeks, new or consistent constipation, and any symptoms associated with weight loss or signs of bleeding should seek help.
New Technology
“There have been several advances in gastroenterology that have transformed the care of patients,” says Tierney. “This includes the development of new combination medications for chronic hepatitis C.”
Previously, hepatitis C was the most common cause of chronic liver disease and cirrhosis in the U.S., and it was difficult to completely eradicate or cure. The treatment plan required injection medications with multiple side effects.
“Now, there are combination pills which can eradicate the virus in six to 12 weeks with very few side effects,” he says. “These medications are so effective that hepatitis C is no longer the most common cause of cirrhosis and the vast majority of patients can be cured.”
For inflammatory bowel disease, new medications are offering improved treatment.
“Even over the last one to two years, there have been numerous medications developed which are more effective at reversing the damage caused by IBD and dramatically altering the quality of life for these patients,” says Tierney.
In addition, he says over the past 10 years, innovation in endoscopic techniques now allows for the removal of cancerous lesions, or the creation of anatomic connections in the digestive tract, that previously were only possible with major surgery.
Colonoscopy Screenings
“For average risk individuals it is recommended to start screening at age 45,” says Tierney.
Tierney says the change in 2018 from screenings beginning at 45 (from age 50) was made due to an increase of colon cancer in younger people.
“The reason for this shift to younger individuals is not clear but has been gradually occurring over several decades and is accelerating,” he says.
Tierney adds that patients with an increased risk of colon cancer based on a family history of colon cancer or the presence of certain bowel diseases should discuss when to start screening with their physicians.
For patients whose colonoscopy results are normal, the recommendation is to repeat the screening in 10 years. However, Tierney says that if the screening reveals polyps, then future colonoscopies will be needed in a shorter time frame based on the number and size of the polyps.
The Bones and Joints
Artificial Disc Replacement
As an alternative to spinal fusion, an artificial disc replacement surgery offers patients more options and greater mobility, according to Kris Parchuri, D.O., an orthopedic surgeon with Tulsa-based Advanced Outpatient Surgery of Oklahoma, as well as Spine and Orthopedic Specialists.
During artificial disc replacement surgery, a herniated or damaged disc is replaced with an artificial disc, unlike a spinal fusion surgery, where the problem disc is removed, replaced with a bone spacer or plastic implant, and then the vertebrae are fused together. Over time, this fused area can begin to cause stress on the vertebrae above and below, which may lead to pain and additional surgeries.
“While fusion surgery limits mobility, patients with a disc replacement can go back to full activities as tolerated,” says Parchuri. “There’s no restrictions; you can get back to the gym or even train as an Olympic athlete.”
Recently, players in the National Hockey League garnered national attention for refusing spinal fusion treatment and opting for artificial disc replacement surgery.
“There’s no set age range,” says Parchuri. “The best candidates are those that typically have one or two level disc problems. It also depends on a person’s activity level and how much arthritis they have in their spine.”
He says recovery time ranges from six to eight weeks and that artificial disc replacement surgery can only be performed in the neck (cervical spine) and the lower back (lumbar spine).
Parchuri says studies with 20 to 25-year data show very minimal wear to the artificial disc.
“As long as it’s put in correctly, there’s no indication that it should not last the rest of your life,” he says.
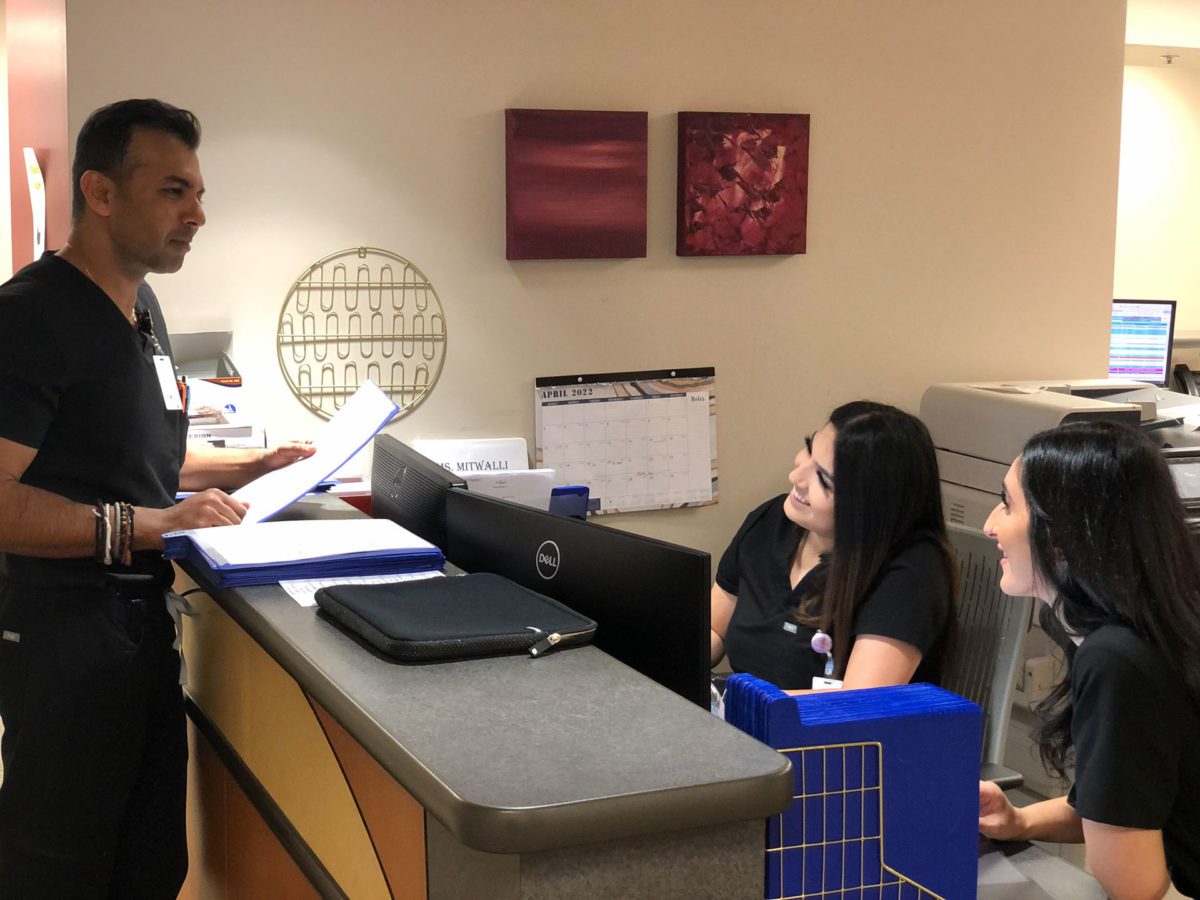
Hip & Knee Surgery and Robotics
“Robotics allows for customization of the implants specific to the patient’s anatomy as well as real-time modifications in surgery,” says Yogesh Mittal, M.D., an orthopedic surgeon with The Orthopaedic Center in Tulsa. “It also allows much more accuracy with less invasive techniques versus manual joint replacements.”
Mittal is currently doing extensive research and development work in the field of robotics to help improve patient outcomes.
“These improvements can allow for better balancing of the ligaments in surgery, along with more anatomic implant positioning,” he says. “Subsequently, patients can recover faster, with less pain and better motion. Next steps include artificial intelligence and machine learning. We have just begun to scratch the surface in this evolving field of robotics.”
He says reported literature suggests that hip and knee replacements last about 12 to 15 years. But “with new and improved current technologies, including robotics, we can expect 25 to 30 years,” says Mittal.
The best candidates for hip replacements are patients who have significant pain in the front crease or side of their hips.
“Oftentimes, these patients have stiffness and loss of motion along with a limp,” he says. “Sometimes they even have limb length discrepancy.”
Individuals in need of a knee replacement may experience knee pain along with stiffness and swelling.
“Oftentimes, they start to lose mobility and lose motion in their knee,” says Mittal. “Both hip and knee patients describe pain with weather changes and stiffness when they first get up from sitting. Prior to surgery, we often try to provide conservative treatments such as NSAIDs, steroid injections and physical therapy.”
Health Tidbits
What is ‘Long COVID’?
“Long COVID is an umbrella term for the wide range of health consequences that are present four or more weeks after infection with SARS-CoV-2,” says Teresa Hardesty, D.O., an internal medicine physician with OSU Medicine in Tulsa. “These symptoms can last weeks, months or years.”
According to the Centers for Disease Control and Prevention, one in 13 U.S. adults are experiencing ‘long COVID’ symptoms.
“Potential symptoms include shortness of breath, exertional intolerance, fatigue, headache, chest discomfort, palpitations, weight loss, difficulty with memory and concentration, anxiety, depression, insomnia, nausea, joint or muscle pain.”
At this time, she says patients who were severely ill and required hospitalization are more likely to have long-term symptoms that last beyond three months. Research is ongoing to determine what risk factors contribute to long COVID, and treatments vary by symptoms.
“For example, patients with post-COVID anxiety or depression can be treated with antidepressant medications and/or counseling,” she says. “Patients with exertional intolerance may benefit from physical therapy, and patients with shortness of breath may benefit from specific inhalers and/or pulmonary rehab.”
While research continues to try and identify the underlying cause of long COVID, risk factors and develop treatments, Hardesty says there are multiple long COVID clinics available to help patients who are struggling with symptoms.
“Oklahoma State University has a long COVID clinic that consists of a multidisciplinary team including internal medicine, pulmonology, cardiology, neurology, psychiatry, physical therapy and osteopathic manipulative medicine,” she says.
IBS vs. IBD
“The most common conditions seen by gastroenterologists include gastroesophageal reflux disease, irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD),” says OU Health’s Tierney. “IBS and IBD are often confused because of the similar acronyms, but they are very different disorders. IBS is more common, and patients typically have abdominal pain associated with either constipation or diarrhea, and importantly, it is not associated with any damage to the intestinal lining. I tell patients the ’S’ in IBS stands for symptoms but no damage, and treatment is designed to improve the symptoms.
“On the other hand, IBD is also associated with abdominal pain and usually diarrhea, but in some patients with Crohn’s disease they may have constipation rather than diarrhea – there is also typically some blood in the stool.”
He says both Crohn’s disease and ulcerative colitis require specialized medications—which may suppress the immune system and require close monitoring for side effects.
“I tell patients the ‘D’ in IBD stands for damage, and the goal of treatment is to heal the damage which will improve symptoms and prevent further complications that can include life-threatening infections or damage that requires surgery,” says Tierney.
Pandemic vs. Endemic
A pandemic recognizes the far-reaching and/or global spread of an infectious disease. The World Health Organization officially declared COVID-19 a pandemic on March 11, 2020. The previous pandemic declaration was in 2009 concerning the novel influenza A (H1N1) virus. Today, questions continue regarding COVID-19 moving into an endemic. As defined by the Centers for Disease Control and Prevention, an endemic “refers to the constant presence and/or usual prevalence of a disease or infectious agent in a population within a geographic area.” Key words attributed to an endemic are stable and predictable. Examples of other endemic diseases include the flu, syphilis and in other parts of the world, malaria. Time will tell if and when COVID-19 reaches an endemic status.
Non-Surgical Eye Treatments
Drs. Do and Tan with Dean McGee say non-surgical rejuvenation, such as injectables and laser therapy, are powerful techniques to accentuate and redefine a patient’s natural appearance.
“Unlike traditional surgery, these techniques are less invasive, have a lower complication rate, and have minimal to no risk of scarring,” says Do. “These procedures can be performed in-office with minimal downtime.”
Botox is the most popular non-surgical rejuvenation procedure, he says.
“The treatment blocks the release of acetylcholine and paralyzes the affected muscles,” says Do. “Strategically placed, injections of botulinum toxin can effectively smoothen wrinkle lines and accentuate certain facial features.”
Tan says resurfacing laser modalities are the best to truly tighten skin but require significant recovery time.
“Not all patients are candidates for all types of procedures, and an in-depth knowledge of the thickness of skin, Fitzpatrick skin type and relative contraindications will identify appropriate candidates,” he says.