By Aisha Patterson and Sarah Teague
Aisha Patterson
During the summer of 2020, I was breastfeeding my 4 month old son when I felt a lump. I breastfed all four of my children, so I assumed it was a clogged milk duct and I ignored it; I told myself that I would get it checked out when I was done breastfeeding.
Four to six months went by and the lump did not go away. In fact, two more appeared, so I finally called my doctor and scheduled an appointment. This was a huge inconvenience to me because I didn’t have health insurance and definitely didn’t think it would be cancer.
After a mammogram, ultrasound and biopsy, I was told that it wasn’t a clogged milk duct. It was invasive ductal carcinoma – stage II, triple positive breast cancer. I was devastated. In November, I began the hardest journey of my life: six rounds of chemotherapy, a double mastectomy and thirty-three rounds of radiation. Having cancer was nothing like I thought it would be – it was a million times worse.
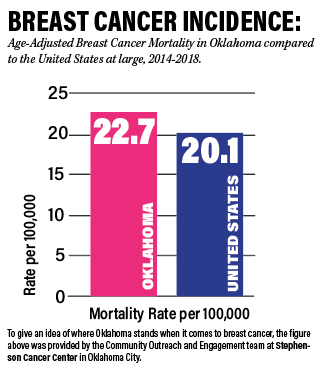
Most breast cancer guidelines in the U.S. cater to women ages 40 and up, yet younger women are being plagued by this disease every day. Cancer is hard at any age, but when a young woman is diagnosed, she faces unique challenges, as she is usually just starting her life, may have young children, or her fertility could be threatened due to chemotherapy. It’s important that women take control of their breast health, no matter their age.
The day after I was diagnosed, I remember walking into my breast surgeon’s office and seeing a sign that said: “Early detection saves lives.”
“Duh,” I thought. Why had I waited so long? At this point, my greatest fear was that the cancer had spread and that I would be facing a stage IV diagnosis, which is incurable. I thought back to every ache and pain I’d experienced over the past 4-6 months and the anxiety washed over me. Why had I not gone to the doctor sooner?
Luckily, my PET scan showed that the cancer did not spread. However, that’s not the case for many women. If I could go back in time, I would have visited the doctor immediately after feeling the first lump. And while I can’t change the past, I now advocate and share my story so other young women will take their breast health seriously.
Breast Health Tips:
1. Get to know your body – specifically your breasts. This will help you to know what’s normal and to identify when something is off.
2. Do a self-breast exam on the first of every month. Put a reminder on the calendar.
3. If you have any of the following changes in your breast, call your doctor as soon as possible: A hard lump; an area that’s thicker than normal; a dimple; nipple crust; a red or hot breast; unexpected fluid; skin sores; bumps; growing veins; a sunken nipple; a new shape/size; or peau d’orange (skin of the breast appearing like the dimpled skin of an orange).
4. Reject the thought that you’re too young to get a breast cancer diagnosis. Instead, take charge of your breast health by being vigilant and reporting any changes that occur. Always get a second opinion if you feel like your concerns aren’t being taken seriously.
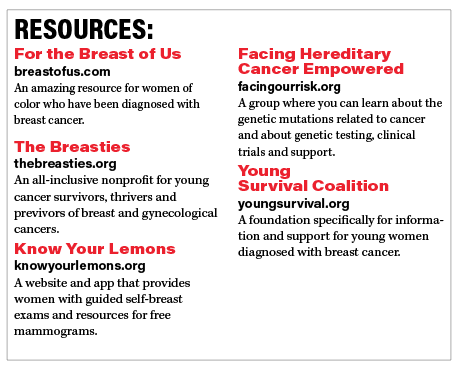
5. If you have a family history of breast cancer, be diligent about check-ups. If you know of a familial genetic mutation, talk to a genetics counselor about being tested for any of the mutations associated with breast cancer.
Sarah Teague
I was five when my mother was first diagnosed with breast cancer. She was 35. She would go on to be diagnosed another two times and pass away from triple negative breast cancer in 2011, at the age of 56. Thus, a good portion of my life was spent at doctor’s appointments and in waiting rooms.
Knowing that I had a family history of breast cancer – as well as my mother having one of the most aggressive forms of said cancer – along with a genetic mutation, it was important for me to get genetically tested. I found out that I also carried the genetic mutation BRCA1, which increased my chances of developing breast cancer to 60-75% during my lifetime. (The general population has around a 13% chance.) So, I made the decision to get a prophylactic double mastectomy in 2016 at the age of 31.
I think it’s important for women to understand that even if I had not had the genetic mutation, my family history was extensive enough for me to advocate for screenings as a younger woman. Some women who find out they have the gene opt to just do surveillance until they decide to pursue surgery or not. It’s a personal decision only you can make. In my particular case, because my mother was diagnosed at a younger age, my doctors felt like surgery was the right decision.
When I hear about women who are on the fence about getting a genetic test because they don’t want to know if they have the gene, my thought is always this: having the knowledge and being proactive, whether that be surgery or consistent screenings, allows you to stay ahead of a potential diagnosis. It allows you to have power over your own health. Once you have a cancer diagnosis, every decision you make is reactionary. To put it another way, let me ask this: If you received a cancer diagnosis, knowing you had the opportunity to avoid it, would you be okay with that?
I understand being proactive can be hard. It means making some very difficult personal sacrifices. And having a genetic mutation doesn’t mean it ends with a double mastectomy; I will have to have screenings and stay vigilant for the rest of my life. I also recognize and am sensitive to the fact that I was able to avoid a breast cancer diagnosis. Some people refer to this as being a “previvor.” And while I don’t love that term, I also certainly don’t call myself a survivor. I am just a young woman who grew up in the cancer world, took what my mother taught me, and make some hard decisions so I could have a different story than hers. I have no doubt that she is relieved to know I listened.