Common Health Risks During Pregnancy
While pregnant, a woman’s body undergoes a multitude of changes, and with these changes come potential health risks. Among the common risks associated with pregnancy are high blood pressure, gestational diabetes, pre-eclampsia and anemia.
In regards to anemia, “thankfully it’s usually a mild complication,” says Kathryn Kramer, MD, an obstetrician-gynecologist (OB/GYN) with OU Health in OKC. “Women are screened for anemia at the start of pregnancy and then again late in the second trimester when they’re also screened for gestational diabetes. If a patient’s blood counts show that they are abnormally low, then we start them on additional iron.”
Screening for anemia is important for several reasons, she says, including monitoring a woman’s overall well-being, how she’s feeling during pregnancy, and in helping to prevent the need for blood transfusions after childbirth.
“During delivery, it’s normal to lose half a liter to a liter of blood depending on the type of delivery,” says Kramer. “If women start out with low blood counts and then lose a significant amount of blood, they are at a higher risk of needing blood transfusions.”
While women who are overweight or obese have a higher risk of developing gestational diabetes or high blood pressure over the course of pregnancy, women at a healthy weight can also develop these conditions, and age can be a factor.
“It’s not fair, but women who are older are at a higher risk for diabetes as well as high blood pressure,” says Kramer. Age 35 and over is considered advanced maternal age and women over 40 have a higher risk of developing hypertensive disorders and gestational diabetes during pregnancy.
“With pre-eclampsia, we have discovered that taking a baby aspirin, an 81 mg tablet, has shown to decrease the chances of developing hypertension and pre-eclampsia during pregnancy,” says Kramer. “We counsel women who have risk factors such as age, weight or prior history to begin taking a baby aspirin along with their prenatal vitamin at around 12 to 13 weeks gestation.”
The Importance of Prenatal Care
Establishing care with an OB/GYN is incredibly important for women of reproductive age, says Kramer, and while prenatal care is essential, it’s also beneficial to be screened for any existing health conditions before becoming pregnant.
Once pregnant, women typically visit their physicians every four weeks during the first two trimesters, every two weeks in the third trimester, and then every week during the last month of pregnancy.
“We’re not only monitoring the baby – checking the baby’s heartbeat – we’re also watching the mother’s weight gain and checking their blood pressure,” says Kramer. “Complications are more likely to develop in the third trimester, which is why we see patients more frequently during the end of pregnancy.”
Food:Kramer encourages her pregnant patients to adopt an overall healthy lifestyle – that yes, you are eating for two, but ‘everything in moderation.’ The average recommended weight gain during pregnancy is between 20 to 35 pounds. However, for someone who is considered obese, the recommendation is between 10 and 20 pounds.
Exercise: “Patients commonly ask if it’s safe to exercise and what they should be doing for exercise,” she says. “Thirty minutes of aerobic activity a day is ideal but, with busy lifestyles, I know that can be challenging. But I find that my patients that exercise regularly tend to feel better throughout their pregnancy and don’t struggle as much with the aches and pains and common discomforts of pregnancy. Our guideline is that anything you were doing comfortably prior to pregnancy is okay to continue, so it’s not recommended to begin a new exercise.”
Caffeine:Many women also worry about being able to still enjoy their morning cup of joe. “I tell patients, don’t deprive yourself. If you need some coffee to stay functional, that’s okay,” says Kramer. During pregnancy, it’s considered safe to drink up to the equivalent of two cups of coffee a day, which is about 120 milligrams of caffeine.
Birth Control 101
Choosing a contraceptive is a personal decision involving many factors including one’s health, lifestyle, potential side effects, efficacy, accessibility and cost.
“Birth control comes in many forms and is not ‘one size fits all,’” says Amber Duncan, APRN, WHNP-BC, with Norman Regional Health System. “Each person can react differently to each type of birth control, so finding the best method for each person can sometimes be challenging.”
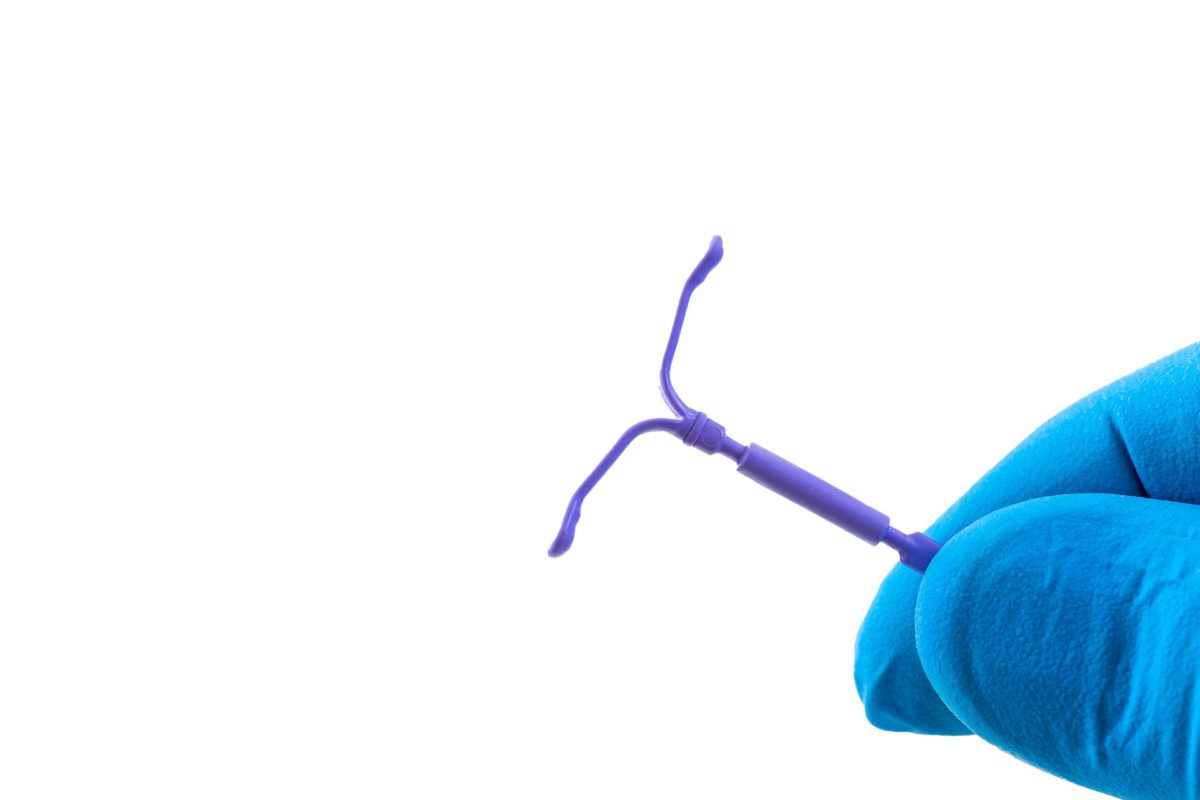
She says in recent years, lower dose oral contraceptives have become popular among patients as well as long-acting reversible contraceptives (LARCs), such as an intrauterine device (IUD) or Nexplanon, a small implant placed in a woman’s upper arm.
“The newest type of birth control to hit the market is a gel called Phexxi,” says Duncan. “This has shown great results so far, and the best part about this form of birth control is that it is hormone free. There are limited choices for non-hormonal birth control, so this is a great new option.”
“If someone has any history of blood clots, stroke, heart attack, or uncontrolled high blood pressure, we would not want to choose anything with estrogen in it,” says Duncan. “Estrogen can increase the risks of these things, making it very dangerous for the patient to be on them. In this case, we would recommend a non-hormonal method or a progesterone-only method such as an IUD.”
She says women who have a family history of breast or ovarian cancer may also choose to stay hormone free and it is typically encouraged.
“It’s important to get feedback from the patient and make an agreed upon decision for what birth control will work out best.”
Low Dose Oral Contraceptives
Efficacy: 99% when taken properly
Pros: Less estrogen exposure than older traditional pills; lighter/shorter menstrual cycles; typically less side effects ie: mood swings, headaches, etc.
Cons: Time sensitive – must be taken within one to two hours of established dosing regimen. (For example, if you choose to take the pill at 9 p.m., then you need to take it within one to two hours of that time each day for it to be most effective.)
IUD (Intrauterine Device)
Efficacy: Over 99%
Pros: Progesterone only, so no estrogen exposure; effective for four to six years dependent upon type of IUD chosen; lighter/shorter menstrual cycles or no cycle at all
Cons: Irregular bleeding, and it can take your body approximately six months to regulate with this device; there is also a risk of the device falling out or migrating.
Nexplanon
Efficacy: Over 99%
Pros: Progesterone only, so no estrogen exposure; effective for three years; lighter/shorter menstrual cycles or no cycle at all
Cons: Irregular bleeding, and it can take your body approximately six months to regulate with this device
Phexxi
Efficacy: 93% when used properly
Pros: Non-hormonal, so only used before intercourse; effective immediately after insertion and good for up to one hour; easy to use and does not require a procedure
Cons: There is the potential for pubic irritation or allergic reaction
Understanding
Sexual Health
A part of being healthy and treating the whole person includes focusing on one’s sexual health. Knowing the difference between a sexually transmitted infection (STI) and a sexually transmitted disease (STD) is a good place to start.
While somewhat self-explanatory by name, an STI is an infection that has yet to develop into a disease, and an STD is a disease, meaning the infection has progressed and is causing more serious problems. Individuals can have infections without it leading to disease, or producing symptoms or long-term health issues.
Roger K. Pfeiffer, DO, an OB/GYN with Ascension St. John Medical Group, says STIs are broken down into three types:
Bacterial: Such as chlamydia, gonorrhea and syphilis
Parasitic: Trichomoniasis
Viral: Herpes simplex virus (HSV), human papilloma virus (HPV), and human immunodeficiency virus (HIV).
“Bacterial STIs are treatable with antibiotics,” says Pfeiffer. “These infections typically present without symptoms, although they can result in abnormal discharge, odor or rash. Long-term and untreated infection can result in sexually transmitted disease such as pelvic inflammatory disease. This is when a bacterial STI has progressed through the fallopian tubes and into the pelvis. For women, this may jeopardize their fertility and increase risk for ectopic pregnancy.”
While syphilis is treated with antibiotics, says Pfeiffer, a person’s screening tests will continue to be positive for the rest of their lives.
“There are many stages of syphilis, but in the absence of routine screening, typically a rash is the first indication of STD,” he says.
“Parasitic STIs are also treated with antibiotics. Trichomonas is a parasitic organism transmitted sexually that typically results in abnormal discharge and odor. HSV is commonly referred to as herpes and is the same virus that causes cold sores (HSV-1), but a different strain (HSV-2) infects the genital region.”
Pfeiffer says HSV typically enters via broken skin and that spot will be the area of future outbreaks, which can begin with some discomfort, tingling, blisters or ulcers.
“Outbreaks tend to be associated with body aches, muscle aches and fatigue with the primary outbreak,” he says. “HSV-1 and HSV-2 can be transmitted to either location, and HSV does not go away and there is no cure. However, there are treatments available to prevent and treat outbreaks.”
Regarding HPV, this sexually transmitted virus can cause genital warts and may cause the development of abnormal cells which can increase one’s risk of certain types of cancer, says Pfeiffer.
“There are more than 100 strains of HPV and roughly half of those can cause abnormal cells that result in pre-cancer and cancer,” he says. “These are called high risk strains. Low risk strains cause warts.”
According to the CDC, more than 9 of every 10 cases of cervical cancer are caused by HPV. For women, a pap test collects cells from the cervix to test for pre-cancerous and cancerous cells. Along with cervical cancer, HPV can also cause cancer in the vagina and vulva. For men, HPV can cause penile cancer and for both men and women, throat and anal cancer.
“There are HPV vaccines that help reduce the likelihood of abnormal cells being caused by infection,” says Pfeiffer. “HPV vaccines are recommended in both young women and young men starting at age nine. The vaccines can be administered up to the age of 45, but it is most beneficial when given before becoming sexually active. Once an infection occurs, a vaccine will not make it go away.”